What is active immunity?
Immunity gained through antibodies received from another individual
Immunity gained after recovering from an infection
Immunity acquired through breastfeeding
Immunity that lasts only a few weeks

Active immunity plays a crucial role in our body’s defense against infectious diseases. This biological process involves the production of antibodies in response to exposure to pathogens such as viruses and bacteria. By delving into how active immunity works, we can better appreciate its importance in maintaining our health and how it forms the basis for vaccines. This explanation will explore the mechanisms of active immunity, its benefits, and its vital role in protecting us from disease.
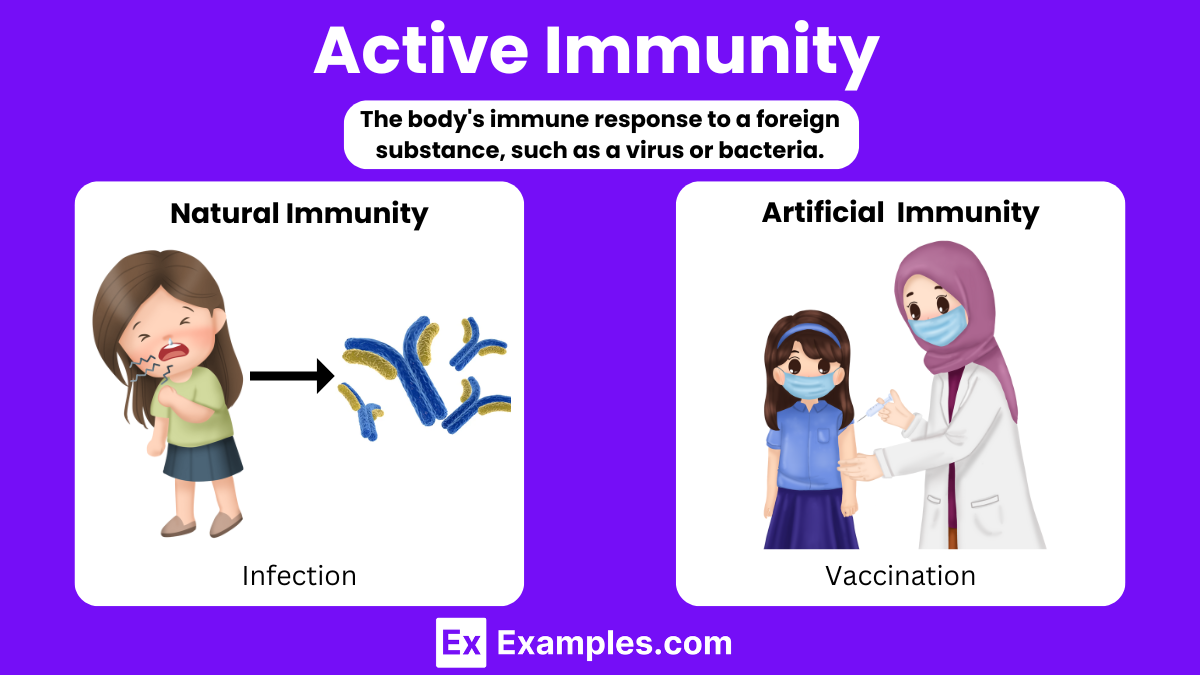
Active immunity is the protection developed when exposure to a disease triggers the immune system to produce antibodies. It can be acquired through natural infection or through vaccination. This type of immunity is long-lasting, and often life-long, providing a rapid response to future exposures to the disease. It can be developed in two primary ways:
Natural active immunity occurs when an individual encounters a live pathogen, develops the disease, and subsequently recovers. During this encounter, the immune system reacts by producing specific antibodies and memory cells. These memory cells ensure the immune system is ready for faster and more effective responses to any future invasions by the same pathogen. For example, once someone recovers from chickenpox, their body usually maintains lifelong immunity against additional chickenpox infections.
Artificial active immunity results from vaccination. Vaccines introduce weakened or inactivated parts of a particular organism (antigen) into the body, triggering an immune response. This immunity aims to mimic an infection, prompting the immune system to produce antibodies and memory cells without causing the full-blown disease. Consequently, if the vaccinated person later encounters the actual disease, their immune system recognizes and responds to it more efficiently. Examples include vaccines for polio, measles, and influenza. This method safely and effectively builds immunity without the individual experiencing the diseases.
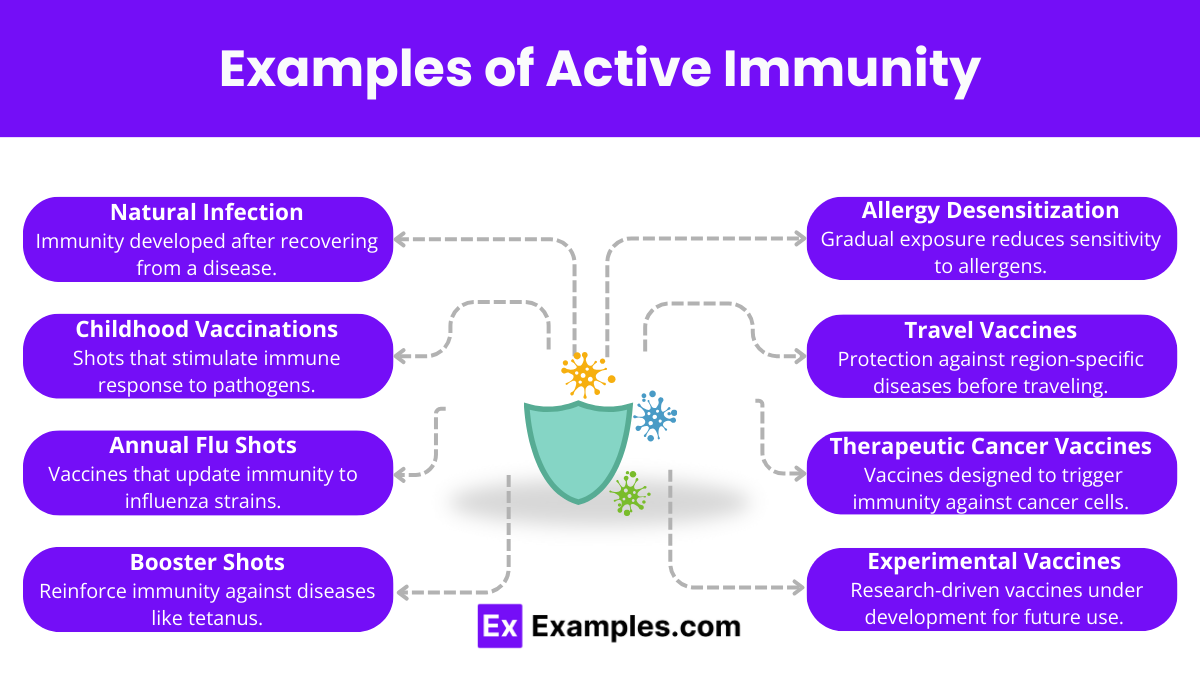
Active immunity is exemplified by a person’s resistance to specific diseases through two primary forms: natural and artificial. Natural active immunity develops when an individual is exposed to a disease organism through infection, leading to the natural production of antibodies. For example, surviving a bout of strep throat naturally triggers the body to build a resistance to future infections by that specific bacterium. On the other hand, artificial active immunity is acquired through vaccination, such as the administration of the polio vaccine, which safely stimulates the immune system to defend against actual infection without causing the disease. Both forms of active immunity are crucial in preventing disease and maintaining public health.
Innate immunity is the first line of defense and is non-specific, meaning it does not target specific pathogens. It includes physical barriers like the skin and mucous membranes, chemical barriers such as acids and enzymes, and cellular defenses like phagocytes and natural killer cells. This type of immunity is present from birth and responds immediately to a wide range of pathogens.
Adaptive immunity develops throughout our lives as we are exposed to diseases or immunized through vaccination. It is highly specific to particular pathogens and consists of two main types:
Passive immunity occurs when a person is given antibodies rather than making them through their own immune system. This can happen naturally, as when a mother’s antibodies are transferred to her baby through the placenta or breast milk, or artificially, through treatments like immunoglobulin therapy or antiserum administration. Passive immunity provides immediate but temporary protection.
Active immunity arises when the body produces its own antibodies in response to the presence of a pathogen. This can be stimulated by natural infection or by vaccination. Active immunity tends to develop over time but offers long-lasting, sometimes lifelong, protection.
The adaptive immune response takes longer to develop than the innate immune response, usually about 1 to 2 weeks to fully work. In contrast, the innate immune system can kick in within twelve hours. A key part of the adaptive immune system is its ability to remember the germs it fights, which can offer lifelong protection against them. Active immunity can happen naturally, like when a child gets and recovers from chickenpox, leading to a specific response to the virus. It can also come from vaccines like the chickenpox shot, which prepares the immune system to fight the disease without causing illness.
Active immunity is a detailed defense system that finds and removes infection-causing germs. This process uses more energy than the initial defenses but kicks in for germs that those defenses can’t handle well. The protection it provides lasts a long time and is important for keeping the body safe from specific germs.
The primary purpose of adaptive immunity is to provide the body with a specialized, targeted defense against specific pathogens, ensuring long-term protection. Adaptive immunity develops as the immune system encounters and responds to foreign invaders like bacteria, viruses, and toxins. It utilizes highly specific immune cells and molecules, such as T cells and antibodies, which recognize and remember specific antigens. This memory allows the immune system to mount a faster and more effective response during subsequent encounters with the same pathogen, often preventing the disease from developing or reducing its severity. Essentially, adaptive immunity is crucial for durable immune protection, allowing individuals to resist repeated infections by the same organism.
Active immunity offers several significant benefits that contribute to both individual and public health:
Active immunity develops from exposure to pathogens or vaccines, lasting long. Passive immunity comes from external antibodies, providing short-term protection.
Passive immunity involves receiving antibodies from another source, offering immediate but temporary disease protection.
Active immunity is immunity formed by the body producing antibodies in response to exposure to an antigen.
Natural active immunity is highly effective as it provides long-lasting protection following recovery from an infection.
Examples of active immunity include recovering from infections like chickenpox or receiving vaccines like MMR (measles, mumps, rubella).
Text prompt
Add Tone
10 Examples of Public speaking
20 Examples of Gas lighting
What is active immunity?
Immunity gained through antibodies received from another individual
Immunity gained after recovering from an infection
Immunity acquired through breastfeeding
Immunity that lasts only a few weeks
Which of the following is an example of naturally acquired active immunity?
Vaccination
Breastfeeding
Getting infected with the flu virus
Receiving a blood transfusion
Which component of the immune system is primarily responsible for active immunity?
Red blood cells
Platelets
T cells and B cells
Plasma proteins
How does a vaccine contribute to active immunity?
By providing temporary antibodies
By introducing dead or weakened pathogens to stimulate an immune response
By directly destroying pathogens
By increasing red blood cell production
Which of the following diseases can be prevented through active immunity via vaccination?
Diabetes
Osteoporosis
Hypertension
Measles
What is the difference between active and passive immunity?
Active immunity is temporary, while passive immunity is long-lasting
Active immunity involves the production of antibodies by the individual, while passive immunity involves receiving pre-formed antibodies
Active immunity is obtained from another person, while passive immunity is self-generated
There is no difference
Which type of cells are responsible for the memory response in active immunity?
Red blood cells
Memory T cells and memory B cells
Platelets
Macrophages
How long does active immunity typically last?
A few days
Several months
Several years to a lifetime
A few weeks
Which of the following statements about active immunity is true?
It can only be acquired through vaccination
It provides immediate protection
It involves the production of antibodies by the immune system
It is less effective than passive immunity
What is the role of booster shots in active immunity?
To enhance and prolong the immune response
To temporarily suppress the immune system
To remove existing antibodies from the bloodstream
To introduce passive immunity
Before you leave, take our quick quiz to enhance your learning!

